How Can I Improve My Sexual Relationship During Menopause?
Improving sleep quality is crucial for overall health. Here are some tips to promote better sleep while going through menopause:
1. Hormone Replacement Therapy
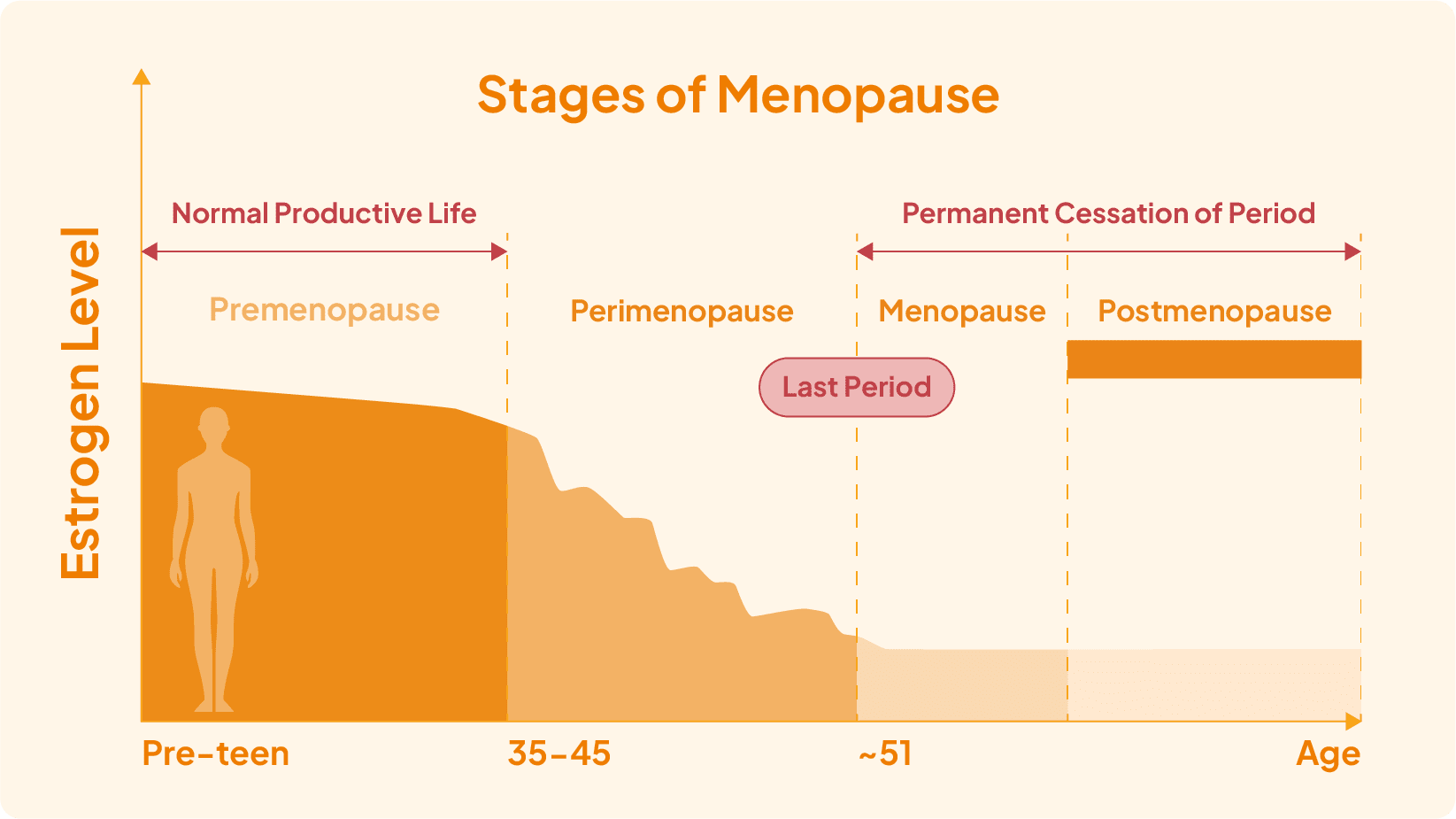
Hormone replacement therapy [10] has improved menopausal women’s sexuality. Both estrogen-only or combined estrogen/progesterone hormone therapy improves women’s sexual desire and overall sexual satisfaction.
Hormone therapy with estrogen can improve sexual satisfaction by improving vaginal secretion and reducing dryness. Estrogen cream or gel for vaginal application can be used to reduce vaginal dryness, however, they are less effective in alleviating hot flashes and night sweating.
Testosterone therapy in addition to women on estrogen hormone therapy may further improve sexual function. Single-use of testosterone therapy might improve sexuality in women who underwent the removal of ovaries.
Conventional estrogen therapy can cause side effects such as heart attack, stroke, blood clot formation and breast cancer. Transdermal estrogen can be considered for safer use.
Hormone replacement therapy should be based on personal needs, preferences, medical conditions, and risk of side effects. It’s best to discuss with a professional while considering hormone replacement therapy.
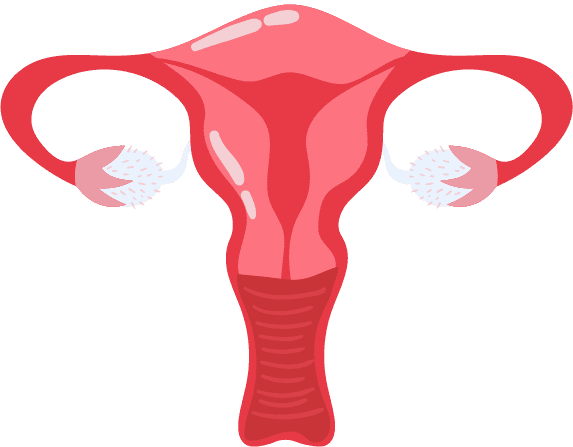
2.Vaginal Lubrication
Water-based or gel-based lubricants can be used to relieve vaginal dryness and reduce discomfort during sexual intercourse.
3.Psychological Counseling
Psychological therapy can be helpful for menopausal women suffering from decreased sexual function. Couples therapy enables couples to improve communication and identify relationship issues.
4.Open Communication
Talking openly with your partner about the changes you are experiencing is crucial for maintaining intimacy during this phase of life.
Many women find it helpful to discuss their changing sexual needs and desires with their partners. With that, both partners can better understand each other’s expectations and work together to find solutions that promote intimacy and pleasure.